[ Download PDF version (203kb) ]
Published in KT Update (Vol. 1, No. 5 - August 2013) [https://ktdrr.org/products/update/v1n5]
An e - newsletter from the Center on Knowledge Translation for Disability and Rehabilitation Research
Dr. Marcel Dijkers, rehabilitation researcher at the Icahn School of Medicine at Mount Sinai, presents another in a series of brief articles around evidence-based research and knowledge translation topics. This article explains the GRADE process (Grading of Recommendations Assessment, Development and Evaluation) and explores its usefulness for rehabilitation and disability research.
Introducing GRADE: a systematic approach to rating evidence in systematic reviews and to guideline development
Marcel Dijkers, PhD, FACRM
Icahn School of Medicine at Mount Sinai, Dept. of Rehabilitation Medicine
GRADE (Grading of Recommendations Assessment, Development and Evaluation) is a well-developed formal process to rate the quality of scientific evidence in systematic reviews and to develop recommendations in guidelines that are as evidence-based as possible. GRADE was developed by an international panel, including members of some of the premier evidence-based practice centers (McMaster, Harvard, the Norwegian and German Cochrane Centres, etc.). While there were some earlier publications,Footnote 1-7 a series of papers published in the Journal of Clinical Epidemiology from 2011 to 2013 constitute the most complete and systematic expose.Footnote 8-22 More information can be found on the GRADE Working Group's website (www.gradeworkinggroup.org).
A number of panels and agencies have adopted GRADE, among others the Cochrane Collaboration (the Effective Practice and Organisation of Care group, the Public Health and other groups), World Health Organization (various guideline development groups), England's National Institute for Health and Clinical Excellence (NICE); the Canadian Task Force on Preventive Health Care, the Norwegian Knowledge Centre for the Health Services, the CDC's Advisory Committee on Immunization Practices, the Kaiser Permanente National Guideline Program, and some groups in the Campbell Collaboration. Some use it with modifications (not recommended by GRADE), and some report minor or major challenges in using the GRADE process unmodified.Footnote 23
GRADE was designed for reviews and guidelines that examine alternative clinical management strategies or interventions, which may include no intervention or current best management. In developing GRADE, the authors considered a wide range of clinical questions, including diagnosis, screening, prevention, and therapy. For that reason, the system can also be applied to rehabilitation, public health, and health systems questions.
GRADE is much more than a rating system, such as those published by various Evidence-Based Practice (EBP) organizations. It offers a transparent and structured process for developing and presenting evidence summaries for systematic reviews and guidelines and for carrying out the steps involved in developing recommendations. GRADE specifies an approach to framing questions,Footnote 9 choosing outcomes of interest and rating their importance,Footnote 9 evaluating the evidence,Footnote 10 including making explicit the risk of various biases,Footnote 11-Footnote 12 and taking into account issues of imprecision (i.e. broad confidence intervals),Footnote 13 inconsistency of results between studies,Footnote 14 and indirectness (i.e. using evidence from a similar population, e.g. stroke instead of traumatic brain injury).Footnote 15
GRADE incorporates evidence with explicit consideration of the values and preferences of patients and society at large to arrive at recommendations. Furthermore, it provides clinicians and patients/clients with a guide to using those recommendations in clinical practice, and policy makers with a guide to their use in health policy.
Based on the recommendations by Johnston and DijkersFootnote 24 for improved evidence standards, a review of a number of existing approaches to systematic reviewing of evidence and developing recommendations (Cochrane Collaboration; Campbell Collaboration, American Academy of Neurology, Centre for Evidence-Based Medicine, among others) likely comes to the conclusion that GRADE is the most flexible methodology with respect to evaluating the evidence (downgrading, upgrading, handling indirect evidence, etc.). It also goes beyond the other systems where it concerns the translation of evidence into recommendations. The special emphasis in GRADE on the values and preferences of consumers (which now is being adopted by others) fits eminently with the traditional emphasis in rehabilitation and disability studies.
The GRADE methodology is applicable whether the quality of the relevant evidence is high or low. The GRADE system was among the first to lay out a systematic way of evaluating whether evidence should be downgraded—for instance, a randomized controlled trial (RCT) executed with poor allocation concealment and high attrition should not be considered to be equivalent to a well-done RCT (see Table 1).
Table 1. Factors that may lead to downgrading or upgrading of evidence in the GRADE approach
| Downgrading |
|---|
|
| Upgrading |
|
In addition, GRADE was the first to specify under what circumstances evidence from a study may be upgraded—for instance, when an effect size is very large, a dose-response gradient is shown, or other circumstances would suggest that what traditionally has been considered a "rather weak design" (e.g. a case-control study) may produce evidence that is of a level produced by an average RCT.Footnote 16
Another advantage of GRADE is that it requires the systematic reviewer to make explicit his or her judgment of each factor that determines the quality of evidence for each outcome. Because alternative diagnostic or therapeutic approaches may all have a balance of positive and negative outcomes (costs, side effects, positive effects in various domains), a guideline developer needs to find a way to systematically identify these, and weigh evidence for all of them simultaneously in making recommendations; GRADE offers a systematic approach to resource useFootnote 17 and to handling multiple outcomes.Footnote 18 Finally, a computer program (GRADEpro) with its associated help file facilitates the development of evidence tables (in GRADE called evidence profiles, or EPsFootnote 19-Footnote 20) and summary of findings (SoFs) tables that are based on the EPs.
Figure 1 presents a schematic view of GRADE's process for developing recommendations; the top half describes steps in the process common to systematic reviews and to guideline development, and the lower half describe steps that are specific to guideline creation. One begins by defining the question in terms of the populations, alternative management strategies (an intervention, sometimes experimental and a comparator, sometimes standard care), and all patient-important outcomes (in this case three). The authors have provided guidance as to which clinical and other questions are suitable for answering with GRADE (or with any systematic review approach, for that matter) and for collecting evidence.
Figure 1. Overview of the GRADE process (modified from Guyatt et al.Footnote 8)
Figure 1 Description
[Select image to enlarge]
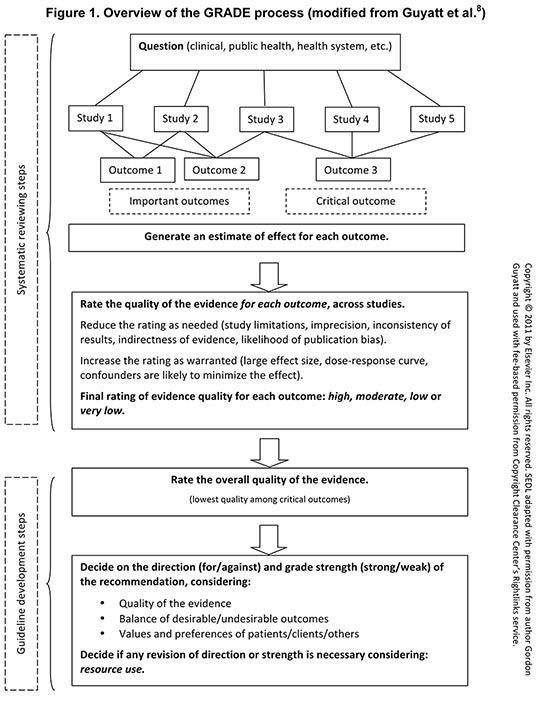
For guidelines, one classifies the outcomes as either critical (one outcome in Figure 1) or important but not critical (two outcomes). A systematic search leads to inclusion of relevant studies (in this scheme, five such studies). Systematic reviewers or guideline authors then use the data from the individual eligible studies to generate a best estimate of the effect on each patient-important outcome and an index, typically a confidence interval (CI), of the uncertainty associated with that estimate.
The Figure illustrates that evidence must be summarized for each patient-important outcome—the summaries ideally coming from optimally conducted systematic reviews. For each comparison of alternative management strategies, all outcomes should be presented together in one EP or SoFs table. It is likely that all studies relevant to a rehabilitation or disability question will not provide evidence regarding every outcome. For example, Figure 1 shows the first study providing evidence for the first and second outcome, the third study for outcomes two and three, and so on. Indeed, there may be no overlap between studies providing evidence for one outcome and those providing evidence for another. For instance, RCTs may provide the relevant evidence for benefits, and observational studies provide the evidence for rare but serious adverse effects.
In the GRADE approach, RCTs start as high-quality evidence and observational studies as low-quality evidence to support estimates of intervention effects. As described above, five factors may lead to rating down the quality of evidence and three factors may lead to rating up (see Table 1). Ultimately, the quality of evidence for each outcome falls into one of four categories from high to very low. Systematic review and guideline authors use this approach to rate the quality of evidence for each outcome across studies (i.e., for a body of evidence). This does not mean rating each study as a single unit. Rather, GRADE is "outcome centric" in that a rating is made for each outcome, and quality may differ—indeed, is likely to differ—from one outcome to another within a single study and across a body of evidence.
Guideline developers (but not systematic reviewers) then review all the information to make a decision about which outcomes are critical and which are important, and come to a final decision regarding the rating of the overall quality of evidence. They next need to consider the direction and strength of recommendation. The balance between desirable and undesirable outcomes and the application of patients' values and preferences determine the direction of the recommendation; these same factors, along with the quality of the evidence, determine the strength of the recommendation. Both direction and strength may be modified after taking into account the resource use implications of the alternative management strategies.Footnote 22
Because most existing systematic reviews do not adequately address all relevant outcomes in a single document, the GRADE process may require relying on more than one systematic review. Systematic reviews often address more than one comparison. They may evaluate an intervention in two disparate populations or examine the effects of a number of interventions. Such reviews are likely to require more than one SoFs table. For example, a review of cognitive remediation may evaluate the effectiveness of training of executive function for different populations, such as those with mild versus moderate traumatic brain injury.
GRADE has been used for a number of systematic reviews and guidelines, including quite a few that would be of interest to professionals with an interest in rehabilitation and disability. Examples: nonpharmacologic interventions for osteoarthritisFootnote 25 and for spasticity in Multiple Sclerosis (MS);Footnote 26 rehabilitation interventions for nonambulatory MS patients;Footnote 27 music interventions for psychological and physical outcomes in cancer;Footnote 28 art therapy for psychosomatic disorders;Footnote 29 exercisesFootnote 30 and manipulationFootnote 31 for chronic neck pain; interventions for depression in the workplace;Footnote 32 parent interventions for children with intellectual disabilities;Footnote 33 childhood adversity as a cause of schizophrenia;Footnote 34 family-based cognitive-behavioral therapy for children and adolescents with obsessive-compulsive disorder;Footnote 35 the benefits of physical activity for youth with developmental disability;Footnote 36 and interventions to enhance return to work by cancer patientsFootnote 37—quite a variety. It may be worth your while to investigate whether GRADE is making the grade.
Footnotes
References
(Select a footnote number to return to that citation in the article.)
- Footnote 1
-
Brozek JL, Akl EA, Alonso-Coello P, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64(5):669-677. doi: 10.1111/j.1398-9995.2009.01973.x
- Footnote 2
-
Brozek JL, Akl EA, Jaeschke R, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 2 of 3. The GRADE approach to grading quality of evidence about diagnostic tests and strategies. Allergy. 2009;64(8):1109-1116. doi: 10.1111/j.1398-9995.2009.02083.x
- Footnote 3
-
Brozek JL, Akl EA, Compalati E, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 3 of 3. The GRADE approach to developing recommendations. Allergy. 2011;66(5):588-595. doi: 10.1111/j.1398-9995.2010.02530.x
- Footnote 4
-
Terracciano L, Brozek J, Compalati E, Schunemann H. GRADE system: New paradigm. Curr Opin Allergy Clin Immunol. 2010;10(4):377-383. doi: 10.1097/ACI.0b013e32833c148b
- Footnote 5
-
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-926. doi: 10.1136/bmj.39489.470347.AD
- Footnote 6
-
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490
- Footnote 7
-
Guyatt GH, Oxman AD, Kunz R, et al. What is "quality of evidence" and why is it important to clinicians? BMJ. 2008;336(7651):995-998.
- Footnote 8
-
Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383-394. doi: 10.1016/j.jclinepi.2010.04.026
- Footnote 9
-
Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol. 2011;64(4):395-400. doi: 10.1016/j.jclinepi.2010.09.012
- Footnote 10
-
Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401-406. doi: 10.1016/j.jclinepi.2010.07.015
- Footnote 11
-
Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). J Clin Epidemiol. 2011;64(4):407-415. doi: 10.1016/j.jclinepi.2010.07.017
- Footnote 12
-
Guyatt GH, Oxman AD, Montori V, et al. GRADE guidelines: 5. Rating the quality of evidence--publication bias. J Clin Epidemiol. 2011;64(12):1277-1282. doi: 10.1016/j.jclinepi.2011.01.011
- Footnote 13
-
Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. 2011;64(12):1283-1293. doi: 10.1016/j.jclinepi.2011.01.012
- Footnote 14
-
Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011;64(12):1294-1302. doi: 10.1016/j.jclinepi.2011.03.017
- Footnote 15
-
Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol. 2011;64(12):1303-1310. doi: 10.1016/j.jclinepi.2011.04.014
- Footnote 16
-
Guyatt GH, Oxman AD, Sultan S, et al. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol. 2011;64(12):1311-1316. doi: 10.1016/j.jclinepi.2011.06.004
- Footnote 17
-
Brunetti M, Shemilt I, Pregno S, et al. GRADE guidelines: 10. Considering resource use and rating the quality of economic evidence. J Clin Epidemiol. 2013;66(2):140-150. doi: 10.1016/j.jclinepi.2012.04.012
- Footnote 18
-
Guyatt G, Oxman AD, Sultan S, et al. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol. 2013;66(2):151-157. doi: 10.1016/j.jclinepi.2012.01.006
- Footnote 19
-
Guyatt GH, Oxman AD, Santesso N, et al. GRADE guidelines: 12. Preparing summary of findings tables-binary outcomes. J Clin Epidemiol. 2013;66(2):158-172. doi: 10.1016/j.jclinepi.2012.01.012
- Footnote 20
-
Guyatt GH, Thorlund K, Oxman AD, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. J Clin Epidemiol. 2013;66(2):173-183. doi: 10.1016/j.jclinepi.2012.08.001
- Footnote 21
-
Andrews J, Guyatt G, Oxman AD, et al. GRADE guidelines: 14. Going from evidence to recommendations: The significance and presentation of recommendations. J Clin Epidemiol. 2013;66(7):719-725. doi: 10.1016/j.jclinepi.2012.03.013
- Footnote 22
-
Andrews JC, Schunemann HJ, Oxman AD, et al. GRADE guidelines: 15. Going from evidence to recommendation-determinants of a recommendation's direction and strength. J Clin Epidemiol. 2013 Jul;66(7):726-35. doi: 10.1016/j.jclinepi.2013.02.003
- Footnote 23
-
Rehfuess EA, Akl EA. Current experience with applying the GRADE approach to public health interventions: An empirical study. BMC Public Health. 2013;13:9-2458-13-9. doi: 10.1186/1471-2458-13-9
- Footnote 24
-
Johnston MV, Dijkers MP. Toward improved evidence standards and methods for rehabilitation: Recommendations and challenges. Arch Phys Med Rehabil. 2012;93(8 Suppl):S185-99. doi: 10.1016/j.apmr.2011.12.011
- Footnote 25
-
Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64(4):465-474. doi: 10.1002/acr.21596
- Footnote 26
-
Amatya B, Khan F, La Mantia L, Demetrios M, Wade DT. Non pharmacological interventions for spasticity in multiple sclerosis. Cochrane Database Syst Rev. 2013;2:CD009974. doi: 10.1002/14651858.CD009974.pub2
- Footnote 27
-
Toomey E, Coote SB. Physical rehabilitation interventions in nonambulatory people with multiple sclerosis: A systematic review. Int J Rehabil Res. 2012;35(4):281-291. doi: 10.1097/MRR.0b013e32835a241a
- Footnote 28
-
Zhang JM, Wang P, Yao JX, et al. Music interventions for psychological and physical outcomes in cancer: A systematic review and meta-analysis. Support Care Cancer. 2012;20(12):3043-3053. doi: 10.1007/s00520-012-1606-5
- Footnote 29
-
Holmqvist G, Lundqvist Persson C. Is there evidence for the use of art therapy in treatment of psychosomatic disorders, eating disorders and crisis? A comparative study of two different systems for evaluation. Scand J Psychol. 2012;53(1):47-53. doi: 10.1111/j.1467-9450.2011.00923.x
- Footnote 30
-
Kay TM, Gross A, Goldsmith CH, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2012;8:CD004250. doi: 10.1002/14651858.CD004250.pub4
- Footnote 31
-
Lin JH, Chiu TT, Hu J. Chinese manipulation for mechanical neck pain: A systematic review. Clin Rehabil. 2012;26(11):963-973. doi: 10.1177/0269215512441485
- Footnote 32
-
Furlan AD, Gnam WH, Carnide N, et al. Systematic review of intervention practices for depression in the workplace. J Occup Rehabil. 2012;22(3):312-321. doi: 10.1007/s10926-011-9340-2
- Footnote 33
-
Einfeld SL, Stancliffe RJ, Gray KM, et al. Interventions provided by parents for children with intellectual disabilities in low and middle income countries. J Appl Res Intellect Disabil. 2012;25(2):135-142. doi: 10.1111/j.1468-3148.2011.00678.x
- Footnote 34
-
Matheson SL, Shepherd AM, Laurens KR, Carr VJ. A systematic meta-review grading the evidence for non-genetic risk factors and putative antecedents of schizophrenia. Schizophr Res. 2011;133(1-3):133-142.
- Footnote 35
-
Gomes JB, Matte BC, Vivan A, et al. Cognitive behavioral therapy with family intervention for children and adolescents with obsessive-compulsive disorder: A systematic review. Revista de Psiquiatria do Rio Grande do Sul. 2011;33(2):121-127.
- Footnote 36
-
Johnson CC. The benefits of physical activity for youth with developmental disabilities: A systematic review. Am J Health Promot. 2009;23(3):157-167.
- Footnote 37
-
de Boer AG, Taskila T, Tamminga SJ, Frings-Dresen MH, Feuerstein M, Verbeek JH. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2011 Feb 16;(2):CD007569. doi: 10.1002/14651858.CD007569.pub2
Suggested citation:
Dijkers, M. (2013). Introducing GRADE: a systematic approach to rating evidence in systematic reviews and to guideline development. KT Update (1)5. Austin, TX: SEDL, Center on Knowledge Translation for Disability and Rehabilitation Research.
KT Update was developed by the Center on Knowledge Translation for Disability and Rehabilitation Research (KTDRR) through grant #H133A120012 to SEDL from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) in the US Department of Education's Office of Special Education and Rehabilitative Services (OSERS). However, these contents do not necessarily represent the policy of the US Department of Education, and you should not assume endorsement by the federal government.
Copyright © 2021 by SEDL.
